58 year old man with Dementia
A 58-year-old, right-handed, married male with a history of alcohol dependence currently in remission over 3 years had presented to our tertiary care rural hospital with a history of onset slurring of speech, urinary incontinence since the past 3 months and significant cognitive decline for 8 months.
He was absolutely alright 8 months back, He was found to carry temple belongings without permission around 8 months back when visiting temples and he incurred the rages of priests and family members and therefore was forbidden to attend the nearby temples.
He had significant forgetfulness for daily tasks, people he met or happenings around and he failed for retrieval of names or objects asked.
On presentation the patient was a thin built middle aged man with stable vitals and who was oriented to time, place but not person. His gait was shuffling. On doing his MMSE score, it came to 6/30. He had a slurred speech though his Comprehension and Repetition were intact. On doing his neurological examination it was found that he was unable to perform the parietal lobar functions.
Speaker Notes:
This graph is from a Randomized placebo controlled trial testing Donepazil in mild to moderate Alzheimer’s patients.
He became reluctant to shave, shower or bathe independently and would need assistance from his son for these tasks. In the ensuing days, he began having difficulty recognizing friends and relatives but would recognize his son and his wife.
He would smile while naming his family members as he could not get their names properly. He sometimes had transient visual and/or auditory hallucinations.
He was unable to button or unbutton his shirt or fold the clothes, unlike his usual self. He repeated the same answer for every question asked (echolalia/ perseverations) and would get impulsive or aggressive about petty issues but also calms down within 5 to 10 minutes on his own as if nothing has happened as he would not remember if being distracted. He, however, stopped laughing at jokes.
For the last 2 months, he had difficulty in swallowing solids and liquids. He showed a remarkable delay in responding to commands, persistent urinary incontinence accompanied by intermittent wandering spells and disinhibited behaviour.
Since 2 months he started complaining of unable to swallow both solids and liquids and he would wet his clothes and complain that he is unable to hold his urine. And when asked a question he would not be able to immediately respond, he sometimes would keep repeating the same words again and again.
VITALS:
BP-130/70mmhg
Pulse-95 bpm
RR-16 cpm
Grbs-146mg/dl
Spo2-98%
GENERAL EXAMINATION:
Patient is a thin built middle aged man
SYSTEMIC EXAMINATION:
CNS--
MMSE
Orientation 1/5
Registration 1/5
Attention calculation 0/5
Recall 0/3
Language
Able to name 2 objects 2/3
Able to repeat no ifs or buts 1/1
Unable to perform 3 steps command 0/3
Patient is unable to read the command to perform it
Patient is illiterate, he is able to write his name 1/1
Total score 6/30
HIGHER MENTAL FUNCTIONS
Patient is conscious, cooperative
He is oriented to person, not time and place
Lobar function tests
Frontal lobe:
Lack of insight to his problems
Unable to perform a series of motor activities
Poor judgement
Unable to perform proverb interpretation test
Parietal lobe:
Ideational apraxia- lost
Right to left orientation-lost
Finger agnosia-present
Unable to perform calculations
Visuo spatial function -lost
Constructional apraxia -lost
Occipital lobe:
Prosopagnosia- Patient is able to recognize only his wife and sons.
Temporal lobe:
Slurred speech
With intact Comprehension and Repetition
Echolalia present
CRANIAL NERVES EXAMINATION
Sense of smell : Intact
EOM Movements: (+)
Pupil Size: Normal
Bilaterally reacting to light
Corneal Reflex:+, jaw jerk -normal
Ptosis: Absent
No deviation of angle of mouth
Nystagmus-absent
Palatal movements - normal
Shrugging of shoulders-Present
No deviation of tongue
Motor System Examination
Tone Upper Limb Lower Limb
Right Normal Normal
Left Normal Normal
Bulk Right Left
Arm 23 cms 23 cms
Forearm 21 cms 21 cms
Thigh 36 cms 36 cms
Leg 26 cms 26 cms
Power
Upper limbs-5/5
Lower limbs-5/5
Hand grip 100% in both sides
Superficial Reflexes
Right Left
Corneal + +
Conjunctival + +
Abdominal + +
Plantar flexor flexor
Deep Tendon Reflexes
Right Left
Biceps 2+ 2+
Triceps 2+ 2+
Supinator 2+ 2+
Knee 2+ 2+
Ankle 2+ 2+
Cerebellar Examination
Nystagmus: absent
Dysdiadokinesia: absent
Finger nose: no incoordination
Sensory System Examination
Pain and temperature sensation-intact
Vibration sense-intact
Joint sense- intact
Gait - Shuffling Gait
CVS - S1,S2 present
Respiratory system - Lungs clear on auscultation
Per Abdomen -
Soft
Non Tender
Bowel sounds present
His Metabolic profile was normal.
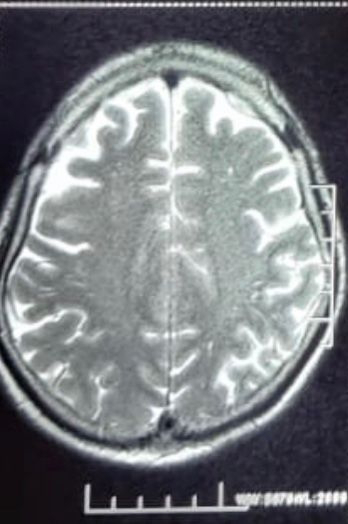
MRI Brain:
Revealed Cerebral and Cebellar atrophy
Chronic ischaemic changes were also noted
T2 weighted image:
T2 weighted image:
Flair Image
Keeping these symptoms of progressive cognitive impairment with impairment of executive, constructive functions, learning, momory a diagnosis of Alzhemiers disease was made and the patient was started on Tab Donepazil 10mg/day which was later increased to Tab Donepazil 20mg/day.
On Followup after 1 month his MMSE declined to 5/30.
Lost follow for 3 months.
3 months later, when asked patients wife regarding the patient's condition we were told that the patient eventually became bedridden and expired 1 month back following aspiration pneumonia.
Discussion:
Speaker Notes:
This is a story of a 58 year old man, who presented to us 2 years back to General Medicine OPD. Let me first tell throw some light into his story. This man used to design sarees at their own tailoring shop and hid wife worked along with him at their tailoring shop along with one among his two sons. His wife told us that he would daily go to the temple every morning and that he also would consume 90ml of whiskey at night after coming back from work atleast for three to four times in a week since the past 10 years. He was apparently absolutely alright 8 months back after which he first noticed that he was finding it difficult to hold the needle while he sat down to design a saree at their shop. He was scolded by his family members for the bad design he made and he was eventually removed from his job by his family as he repeatedly failed to design the sarees like before. He started staying at home without looking for another job and would feel sad that he couldn't contribute to his family's business. A month later his wife found temple idols hidden in his pockets and when questioned about it the patient denied. This act of his kept getting repeated, his wife repeatedly found temple idols in his pockets and he would get scolded by his family members but the patient continued. He was abandoned from nearby temples. He also started to hide his clothes in various places.
6 months later they noticed his speech became slurred and he stopped dressing properly or even combing his hair. Thinking this was part of his negligence, he was scolded by his parents, wife and sons. But he continued. He would also hide his clothes in hidden places. When questioned about it he would deny it. Since 4 months he wasn't able to recognize his friends and would isolate himself and not get involved into conversations. He slowly started to forget names of his family members.
He started to complain to hear voices or seeing a snake
3 months back his wife was told by their neighbor that he was seen roaming on the streets of their colony shirtless. He was immediately brought back to home and was scolded. He however would continue the same when noone was at home to look after.
This was when the patient presented to us with his wife and son. As that's when their family realized he could be having a medical problem.
He also started to complain about a snake roaming in his room
No other neurological deficit was found. His metabolic profile was normal.
On neuroimaging his mri brain reveled cerebral and cerebellar changes with chronic ishaemic changes.
Speaker Notes:
These are the learning objectives that you'll be able to take home after this presentation. I'll be talking about the approach to dementia and how to differentiate and clinically decide the type of dementia. And a little bit about memory. I'll also talk about Alzheimer’s disease, the diagnostic approach and the therapeutic efficacious.
Speaker Notes:
So how do you approach dementia. First after a detailed history, we need to rule out pseudodementia and if it is a dementia is it cortical or subcortical and what are the lobes involved. We need to rule out the reversible cause of dementia before thinking about the irreversible causes.
Speaker Notes:
So what exactly is dementia and how would you define it by the DSM 5 (The diagnostic and statistical manual of mental disorders).
It is the development of multiple cognitive defects including memory and one or more of the following cognitive domains :
1. Complex attention
2. Executive function
3. Learning and Memory
4. Language
5. Motor or Social Cognition
And also the decline of cognition noted by the clinician or the informant and also documented impairment in the patients cognition noted by a standardized neuropsycholocial testing.
The cognitive decline not explained by delirium or other mental disorders such as Schizophrenia or depressive disorder.
Speaker Notes:
So what is the difference between Dementia and Pseudodementia? What is exactly pseudodementia?
Patients with pseudodementia have a rapid progression unlike the slow progression seen in dementia along with a more frequent psychiatry history and high suicidal tendencies. When asked they would respond 'I do not know' or 'I do not want to answer' and they would have insight.
Speaker Notes:
So before going into Dementia, i would like to talk briefly about memory and where it is stored.
There are three types of memory, the immediate, recent (short term memory) and remote memory which is the long term memory.
The immediate memory is stored in the reticular activating system. Short term memory in the hippocampus.
The long term memory could be explicit or non explicit. The explicit could be semantic - which includes information or knowledge stored in the cortical association areas or the episodic memory stored in the medial temporal.
Implicit memory includes procedural skills, priming, conditioning.
Speaker Notes:
So, How do you differentiate if it is a cortical or a subcortical Dementia?
As the name suggests cortical dementia involves the cortical whereas the subcortical involves the subcortical grey matter. You can by the name understand what symptoms could be expected when each of this is involved.
When the cortex is involved you would expect the patient to have - lack of insight, behavioral changes, aphasia, parietal lobar impairment with rarely involvement of the motor system. The subcortical dementia usually would have more motor complains.
Speaker Notes:
This slide shows the individual lobar functions which would help us analyze which part of the brain is involved.
For example in our patient, his judgement, executive functions is impaired along with behavioral changes would point more towards the involvement of parietal lobe and the Frontal lobe.
Speaker Notes:
Some of the reversible causes of dementia are hypothyroidism, thiamine deficiencies, vitamin B12 deficiency, drugs such as benzodiazepines.
Where as the irreversible causes are Alzheimer’s disease being the most common form of dementia, Frontotemporal dementia, Parkinson's disease.
Alzheimers accounts for 50 to 75 percent of Alzheimer’s disease followed by Vascular dementia.
Speaker Notes:
These slides help us to differentiate the irreversible causes of dementia.
The Alzheimer’s disease usually has a gradual progression of cognitive dysfunction in comparison to the Vascular dementia which has a more abrupt progression and with focal neurological deficits. Patient with Frontotemporal dementia usually manifest with disinhibitio, more of a behavioral changes, the patient would be unable to perform the Frontal lobar tests such as sequencing, planning.
Alzheimer's disease can be differentiated from parkinsions disease as it doesn't usually have motor symptoms.
One interesting question was asked to me about my case a few days back - why couldn't this be CJD ?
CJD usually is a rare prion disease and is a rapidly progressive disorder with the life expectancy being around 2-3 years. However most of the patient's die weeks to months after initial symptoms. These patients usually also present with myoclonus, involuntary movements.
So what is Alzheimer’s disease?
1906, the German psychiatrist and neurologist Dr Alois Alzheimer first identified the illness that would become known as Alzheimer's disease. His discovery was based on the case of a 51-year-old woman, Auguste Deter, who had suddenly begun to exhibit irrational behaviour and memory loss.
Speaker Notes:
So how do you diagnose Alzheimer’s disease?
According to DSM 5 these following criteria need to be met to call it Alzheimer's Disease
A. Criteria are met for major or mild neurocognitive disorder.
B. There is insidious onset and gradual progression of cognitive impairment, for the major neurocognitive disorder atleast 2 domains must be impaired.
For major neurocognitive disorder:
1. Alzhemier's disease genetic mutation from family history or genetic testing.
2. All the three of the following are present:
1) Clear evidence of decline in memory and learning or any other cognitive domain.
2) Steadily progressive, gradual decline
3) No evidence of mixed etiology
Minor criteria involves no evidence of possible genetic mutation in the family or from genetic testing.
Speaker Notes:
In a meta analysis done by Barnes in 2011, the relative risk of diabetes mellitus to Alzheimer’s disease was found to be 1·47. Another 4 meta analysis studies also showed a significant association of diabetes to dementia. Other namely risk factors were Hypertension, Smoking, Low education, obesity.
Midlife Hypertension to Alzheimer’s dementia was found to have a relative risk of 1.61 by Barnes and his colleagues.
The probable association of age to Alzheimer’s dementia could be explained by the Nun study, where in the brain autopsy of a cognitively perfect nun at 101 years showed neurofibrillary tangles. I would like to talk more on this study in the ending of our presentation.
Another study concentrated on the relation between leisure activities and Dementia.
469 subjects were included of 75 to 85 years old. These participants were involved in follow-up period of 5.1 years. These patients were involved in leisure activities of , reading, playing board games, playing musical instruments, and dancing, along with physical activities. Participants who were involved in leisure activities were associated with a reduced risk of dementia.
Speaker Notes:
These are the seven stages of Alzheimer’s disease according to the FAST scale.
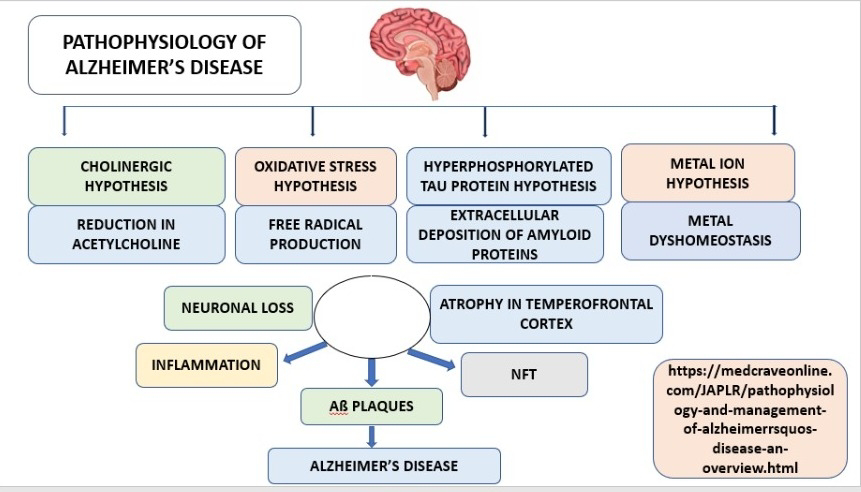
There a number of pathways hypothesized in the pathophysiology of Alzheimer's Disease.
The cholinergic hypothesis states that the reduction in acetylcholine in the brain is the pathogenesis behind Alzheimer’s disease. This is the reason why Acetylcholinesterase inhibitors are given for treating these patients.
Tau hyperphosphorylation : Increase in intracellular tau accumulation induces multiple cellular impairments, including endoplasmic reticulum stress, deficits of mitophagy and autophagy, deficits of synaptic transmission, etc., and eventually leads to a chronic neurodegeneration.
There is a metal ion hypothesis, Iron accumulation in the brain is thought to be the cause of several neurodegernative disorders.
Speaker Notes:
Some of the genes associated with Alzheimer’s disease are - Apo E4, Presenting 1, 2 which could be tested by genetic testing.
Neuroimaging won't be very useful at the early stages of the disease but in the later stages a posterior predominant cortical atrophy, medial temporal atrophy could be found.
Hypometabolism in the posterior temporal parietal cortex could be present on the PET Scan.
CSF Analysis may show low alpha beta amyloid levels and high phosphorylated tau levels.
EEG is usually normal or non specific.
Speaker Notes:
Do these investigations really confirm the diagnosis?
This is a story from a sister who shares her brother's journey in finding the definitive diagnosis for his neurological disease. He was first diagnosed with Parkinson's Disease, Multi System Atrophy after undergoing a number of investigations including MRI Brain, PET Scan but always received a different diagnosis with a different physician. After his death, his brain autopsy revealed lewy body disease with brain stem predominance.
We actually really need more people like her, as it's really important to know the diagnosis of any disease and it is important to know the cause by doing a brain autopsy that would help us further come closer to the diagnosis when a similar patient presents.
Speaker Notes:
Acetylcholinesterase inhibitors act by preventing the break down of Acetylcholine in the brain. Some of these namely drugs are Donepezil, Galantamine, Rivastigmine. Donepezil is the most commonly used drug.
An N methyl D aspartate antagonist which blocks toxic effects associated with excess glutamate. Memantine could be used as well for moderate to severe dementia. Though few studies favour the use of memantine whereas others don't find it to be beneficial.
P - 286 patients were included in this study
I - Donepezil (n = 142; 5 mg/day for 28 days, followed by 10 mg/day)
C - placebo (n = 144) for 1 year
O - The cognition of the patients were assessed at 24, 36,52 by MMSE , Progressive Deterioration Scale. A improvement in patients cognition were observed in patients on Donepezil.
Speaker Notes:
P- One hundred twenty older adults without dementia.
I - The exercise group included 60 participants.
C - The stretching control group included 60 participants.
O - Magnetic resonance images were collected before the intervention, after 6 months, and again after the completion of the program. The aerobic exercise group demonstrated an increase in volume of the left and right hippocampus, whereas the stretching control group displayed a decline over this same interval.
Speaker Notes:
Intracerebral transplantation of Bone Marrow –Mesenchymal Stem cells into APP/PS1 mice significantly reduced amyloid β-peptide (Aβ) deposition. Furthermore, APP/PS1 mice treated with BM-MSCs had decreased tau hyperphosphorylation and improved cognitive function.
Not in Favour:
One study showed that there were no benefits from Bone Marrow stem cell transplant where as some studies reported increase in the level of Amyloid plaques in the mice brain and behavioral abnormality.
Speaker Notes:
Adrian et al included 6 patients with Alzheimer’s disease who received continuous deep brain stimulation got 12 months. MMSE showed improvement at 6 and 12 months.
However this is a case report of a patient who reportedly developed Bilateral encephalomalacia after deep brain stimulation.
And the ADVANCE study conducted on 42 participants with Alzheimer’s disease - 26 patients experienced adverse effects where as 5 patients experienced serious adverse effects such as infection, subdural hematoma. 4 patients required to return to surgery.
Speaker Notes:
These patients would require a caregiver but caregiver burden, caregiver distress were highly reported.
Many studies have reported cognitive improvement after cognitive rehabilitation especially at the early stages. The reference here is about a study where in 52 patients were included in the study and a slight reduction of the cognitive impairment was noted, however there was reduction of caregiver burden, as the participants were involved in various leisure activities.
It would be further helpful to further expand our clinical knowledge if we further practice case based blended learning and discussion.
Speaker Notes:
A significant association of aspiration pneumonia has been associated with Alzheimer’s disease similar to our patient. A study observed out of 25 patients with Alzheimer’s disease 6 patients developed aspiration pneumonia.
In the Nun study,
"We need more people like Sister Mary who are
willing to make such sacrifices. Sister Mary did not directly benefit from participation in the Nun Study, but her friends and family knew that she felt better for doing it.
She was willing to lay out her life, her
cognitive function, and her brain in all their details. Her only request was that we simply refer to her as Sister Mary. She did not want to become a celebrity. She did not want the accolades."
We need more people like Sister Mary that are willing to help us for the betterment of Medicine and science as there is still a lot that is unknown.

































Comments
Post a Comment