A 50 year old woman presented to our OPD with the complaints of
Lower back pain since the past 3 months
Forgetfulness since 3 months
Slurring of speech since 3 months
She was born out of a non consanguinous marriage. She never attended school. She got married to a farmer when she was 16 years of age. She had three normal vaginal deliveries (2 daughters and a son). She used to work as a farmer along with her husband.
6 years back when she was working at a paddy field, she came in contact with electric shock for which she was admitted for 2 days in a local hospital. She had no complaints back then except for generalized weakness. She was given IV fluids during her hospital stay. She stopped going to work after this incident.
1.5 years back she again came in contact with electric shock when she was working at her house.
3 months back when she was walking to the washroom , she had a fall and injured her lower back. Ever since then she has been complaining of lower back pain.
Her daughter tells us that her mother has been experiencing frequent falls since the past 3 months.
She also tells us that she previously used to be a very friendly person, who maintained good relations with their neighbor's, relatives. She would often worry regarding their financial situation and would frequently quarrel with her husband regarding starting their own business. Her daughter also told us that when her brother decided to move out with his wife, his mother was against it and ever since he moved out she has been low.
Over the past 3 months, her daughter reports that her mother has gradually stopped interacting with others. She doesn't like meeting her relatives, friends. She also frequently has anger outbursts with no triggers where she starts yelling but there are no reports of throwing objects in anger. She also tells that she would randomly start crying without any reason.
She reports that since the last month she is unable to recognize her relatives or neighbours. She only recognizes her family members. Her daughter also tells us that she occasionally passes urine and stools in her clothes and when scolded she starts crying.
Her daughter also reports that she now doesn't know her way home without proper guidance.
She used to previously cook for her family but now she isn't able to cook. She is unable to eat on her own, take shower or get dressed without help. She is unable to perform her routine daily activities without any help.
20 days back, she had one episode of seizure which lasted for 15 minutes, consisted of tonic posturing of all her limb, uprolling of eyes, froth discharge from mouth which was followed by post-ictal confusion which lasted for 20 minutes. She had a similar episode 1 week back
She is a thin built woman
Pallor +
Lack of facial expressions while conversing
On nervous system examination:
Right handedness
She did not attend school
Higher mental functions:
Right handedness
MMSE: 13/30
Appearance : Not well dressed
Level of consciousness: 15/15
Speech : Not fluent, comprehension intact, repetition intact
Cranial Nerves intact
Sensory System intact
Motor System:
Cerebellar signs intact
Lobar function tests:
Frontal lobe:
Her sense of dressing and behaviour - also goes in favour of frontal lobar involvement
Able to perform motor luria test - fist edge palm test
Luria graphic test -
Unable to perform stroop test
Parietal lobe:
Right to left oriental lost
Visuo-spatial orientation lost
Unable to perform simple and complex calculations
Geographical disorientation
Temporal lobe:
Memory lost
Occipital lobe:
Prosopagnosia lost
Loss of visual memory
Autonomic System:
Orthostatic Hypotension present
Cardivascular System Examination:
Apex beat in 5th intercostal space, 0.5cm medial to midclavicular line
S1,S2+
Pansystolic murmur + in Mitral area
Other System Examinations - Normal
Provisional Diagnosis:
Alzheimer's Disease
Vascular Dementia
Speaker notes for slide 1:
Good morning everyone
I’m Dr Aashita, senior resident from the department of general medicine
Today I’ll be discussing about my field of interest that is the neurodegenerative disorders and some of such cases I’ve seen during my residency and my senior residency.
First I’ll be presenting a case of a 50 year old woman with dementia and other symptoms.
Will be elaborating on the history
Speaker notes:
Tone and Power of all the four limbs are normal.
Reflexes - All her reflexes are exaggerated. Plantars - Mute bilaterally
Sensory system - Intact
Cranial nerves - Intact
Speaker Notes: These are frontal lobe tests
Also her sense of dressing and behaviour - also goes in favour of frontal lobar involvement
Parietal lobe tests - she wasn’t able to differentiate between right and left
Unable to make out right and left discrimination
Visuospatial orientation lost
Geographical orientation lost
Unable to perform simple calculations
Temporal lobe involvement :
Slurred speech with intact comprehension and repetition
Memory -
Occipital lobe :
We check for prosopagnosia and visual memory which are lost
She was able to perform the motor Luria test that is the first edge palm test
But the luria graphic test she wasn’t able to perform as shown here for frontal lobe
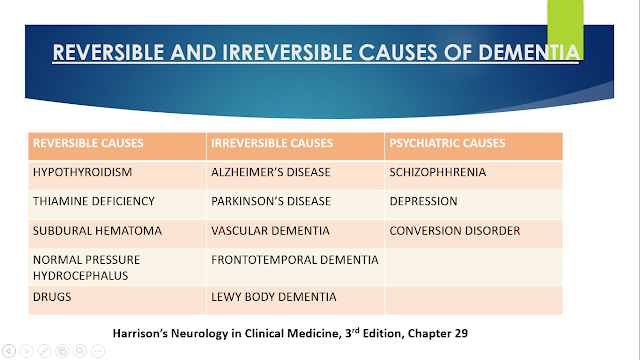
Speaker Notes: These are my differentials. However Alzheimer's disease is a gradually progressive disease whereas lewy body dementia is of rapid onset. Vascular dementia is of sudden onset with focal neurological deficits. In lewy body dementia patients usually present with fluctuating memory & hallucinations, In frontotemporal dementia patients behaviour & execution is affected. So lets further go into details of dementia prior to coming to a diagnosis.
Speaker Notes:
These are the learning objectives that you'll be able to take home after this presentation. I'll be talking about the approach to dementia and how to differentiate and clinically decide the type of dementia. And a little bit about memory. I'll also talk about vascular dementia, the diagnostic approach and the therapeutic efficacies.
Speaker Notes:
So how do you approach dementia. First after a detailed history, we need to rule out pseudodementia and if it is a dementia is it cortical or subcortical and what are the lobes involved. We need to rule out the reversible cause of dementia before thinking about the irreversible causes.
Speaker Notes:
So what exactly is dementia and how would you define it by the DSM 5 (The diagnostic and statistical manual of mental disorders).
It is the development of multiple cognitive defects including memory and one or more of the following cognitive domains :
1. Complex attention
2. Executive function
3. Learning and Memory
4. Language
5. Motor or Social Cognition
And also the decline of cognition noted by the clinician or the informant and also documented impairment in the patients cognition noted by a standardized neuropsychological testing.
The cognitive decline not explained by delirium or other mental disorders such as Schizophrenia or depressive disorder.
Speaker Notes:
So what is the difference between Dementia and Pseudodementia? What is exactly pseudodementia?
Patients with pseudodementia have a rapid progression unlike the slow progression seen in dementia along with a more frequent psychiatry history and high suicidal tendencies. When asked they would respond 'I do not know' or 'I do not want to answer' and they would have insight.
Speaker Notes:
So before going into Dementia, i would like to talk briefly about memory and where it is stored.
There are three types of memory, the immediate, recent (short term memory) and remote memory which is the long term memory.
The immediate memory is stored in the reticular activating system. Short term memory in the hippocampus.
The long term memory could be explicit or non explicit. The explicit could be semantic - which includes information or knowledge stored in the cortical association areas or the episodic memory stored in the medial temporal.
Implicit memory includes procedural skills, priming, conditioning.
.png)
.png)
Speaker Notes:
So, How do you differentiate if it is a cortical or a subcortical Dementia?
As the name suggests cortical dementia involves the cortical whereas the subcortical involves the subcortical grey matter. You can by the name understand what symptoms could be expected when each of this is involved.
When the cortex is involved you would expect the patient to have - lack of insight, behavioral changes, aphasia, parietal lobar impairment with rarely involvement of the motor system. The subcortical dementia usually would have more motor complains.
.png)
This slide shows the individual lobar functions which would help us analyze which part of the brain is involved.
For example in our patient, his judgement, executive functions is impaired along with behavioral changes would point more towards the involvement of parietal lobe and the Frontal lobe. Unusual emotions, prosopagnosia, unable to recognize relatives & friends points towards involvement of temporal and occipital lobes.
Some of the reversible causes of dementia are hypothyroidism, thiamine deficiencies, vitamin B12 deficiency, drugs such as benzodiazepines.
Where as the irreversible causes are Alzheimer’s disease being the most common form of dementia, followed by vascular dementia which is the second most common cause, Frontotemporal dementia, Parkinson's disease.
Speaker Note:
Alzheimers accounts for 50 to 75 percent of Alzheimer’s disease followed by Vascular dementia.
.png)
.png)
Speaker Notes:
These slides help us to differentiate the irreversible causes of dementia.
The Alzheimer’s disease usually has a gradual progression of cognitive dysfunction in comparison to the Vascular dementia which has a more abrupt progression and with focal neurological deficits. Patient with Frontotemporal dementia usually manifest with disinhibition, more of a behavioral changes, the patient would be unable to perform the Frontal lobar tests such as sequencing, planning.
Alzheimer's disease can be differentiated from parkinsions disease as it doesn't usually have motor symptoms.
Speaker Notes:
MRI brain - First image is FLAIR showing periventricular hyperintensities suggestive of small vessel ischemic disease
Next two images are ADC and last is DWI showing diffusion restriction in corona radiata and right parietal region suggestive of acute infarct
Speaker Notes:
Xray Lumbo-sacral spine showing reduced vertebral body height.
Old T11 fracture with diffuse osteoporosis for which orthopedics opinion was taken. Advised pain relieving medications and MRI Lumbo-sacral spine.
Speaker Notes: Alois Alzheimer is best known for his description of neurofibrillary changes in brain neurons of a demented patient. Biswanger addressed heterogeneity of dementia syndromes by delineating vascular dementia from syphilitic dementia and Alzheimer best understood the cause for dementia
Speaker Notes: Will be discussing the following table orally
From uptodate
Speaker Notes: Some of the risk factors are hypertension, diabetes, age, stroke, metabolic syndrome, genetic factors
Speaker Notes:
Using the KoreanService-Health Screening Database from 2009 to 2012, a total of 4 522 447 adults aged 60+ years without a history of dementia were analyzed and followed up for a mean of 5.4 years. Individuals were classified according to their baseline systolic BP (SBP) and diastolic BP; SBP 130 to <140 mm Hg and diastolic BP 80 to <90 mm Hg were used as reference groups. The risk of overall dementia and probable Alzheimer disease was significantly higher in the SBP≥160 and lower SBP groups.
Probable AD and probable VaD occurred in 219 562 (4.8%) and 37 076 (0.8%) of participants, respectively
Diabetes mellitus and risk of dementia: A meta-analysis of prospective observational studies
The present meta-analysis of 28 observational studies showed a 73% increased risk of ATD, 56% increase in AD and 127% increase in VaD in patients with history of diabetes as compared with non-diabetic people.
469 subjects were included of 75 to 85 years old. These participants were involved in follow-up period of 5.1 years. These patients were involved in leisure activities of , reading, playing board games, playing musical instruments, and dancing, along with physical activities. Participants who were involved in leisure activities were associated with a reduced risk of dementia.
7528 participants of the Rotterdam study aged 55-106 years.
474 cases of dementia were detected, giving an overall prevalence of 6.3%.
Alzheimer's disease was the main subdiagnosis (339 cases; 72%). The relative proportion of vascular dementia (76 cases; 16%), Parkinson's disease dementia (30; 6%), and other dementias (24; 5%) decreased with age.
Speaker Notes: The pathology behind vascular dementia are due to large vessel diseases with multiple infarcts, single infarct, small vessel diseases showing multiple lacunar infarcts, ischemic white matter change, microinfarcts/ microhemorrhages or any hemorrhage like intracerebral hemorrhage, subarachnoid hemorrhage., hypoperfusion.
This could be due to any atherosclerosis, vasculitis, emboli.
Speaker Notes; Pathogenesis of vascular dementia is such that a Small vessel disease, thromboembolism or hypoperfusion of the brain leads to reduced cerebral blood flow leading to hypoxia, oxidative stress, inflammation further leading to white matter damage such as demyelination, neurodegeneration, neuroinflammation which eventually leads to cognitive decline, vascular dementia.
Speaker Notes: Clinically vascular dementia could be diagnosed by the presence of focal neurological deficits, abrupt onset and fluctuating memory. It could be assessed clinically by cognitive assessments like the mini mental state examination or montreal cognitive assessment. Imaging that is MRI brain full filling vascog criteria.
Speaker Notes: Hachinski ischemic score is a cognitive assessment so in this assessment either 2 points or 1 point is given. If the patient has an abrupt onset of symptoms, fluctuating memory, focal neurological symptoms or signs you give 2 points. For patients with hypertension, depression, personality changes, associated atherosclerosis 1 point is given.
A score less than 4 is indicative of Alzheimer's dementia
7 or more is indivative or vascular dementia. Our patients score was 8.
Speaker Notes: This is the montreal assessment chart which consists of identifying the animal (naming), visuospatial execution, memory by naming different words such as velvet, church and asking the patient to repeat it, attention, calculation and orientation similar to MMSE.
Speaker Notes: Efficacy and Tolerability of Donepezil in Vascular Dementia
P = 603 with probable (70.5%) or possible (29.5%) VaD, according to criteria of the National Institute of Neurological Disorders and
Stroke
I = 24 weeks of treatment with donepezil 5 mg/d (n=198), donepezil 10 mg/d (5 mg/d for first 28 days; n=206)
C - Placebo (n=199)
O - At week 24, both donepezil groups showed significant improvement in cognition versus placebo on the Alzheimer’s Disease Assessment Scale–cognitive subscale
Donepezil-treated patients showed significant benefits in activities of daily living over placebo on the Alzheimer’s Disease Functional Assessment and Change Scale
Speaker Notes: P - A total of 548 patients with vascular dementia were included in the study
I - 277 patients who were receiving memantine
C - 271 patients who were receiving placebo
O - No significant difference was noted between memantine and placebo group
Speaker Notes: Studies have shown that patients with type 2 Diabetes Mellitus on Metformin had lower incidence of dementia.
Propentofylline:
Pathophysiologic processes common to both vascular dementia and dementia of the Alzheimer type may include microglial activation with resultant generation of inflammatory cytokines and neurotoxic free radicals, decreased secretion of nerve growth factor by astrocytes, excess release of glutamate with associated neurotoxicity, and loss of cholinergic neurons. The functional benefits and neuroprotective effects of propentofylline (PPF) stem from its interference with these overlapping pathways of neurodegeneration.
It was found to be beneficial in clinical 2 trial.
Speaker Notes: 1409 individuals - followed up for 21 years. 61 cases were diagnosed with dementia (48 with Alzheimer’s disease). Coffee drinkers at midlife had lower risk of dementia and Alzheimer's disease later in life compared with those drinking no or only little coffee.
Speaker Notes:
These patients would require a caregiver but caregiver burden, caregiver distress were highly reported.
Many studies have reported cognitive improvement after cognitive rehabilitation especially at the early stages. The reference here is about a study where in 52 patients were included in the study and a slight reduction of the cognitive impairment was noted, however there was reduction of caregiver burden, as the participants were involved in various leisure activities.
It would be further helpful to further expand our clinical knowledge if we further practice case based blended learning and discussion.
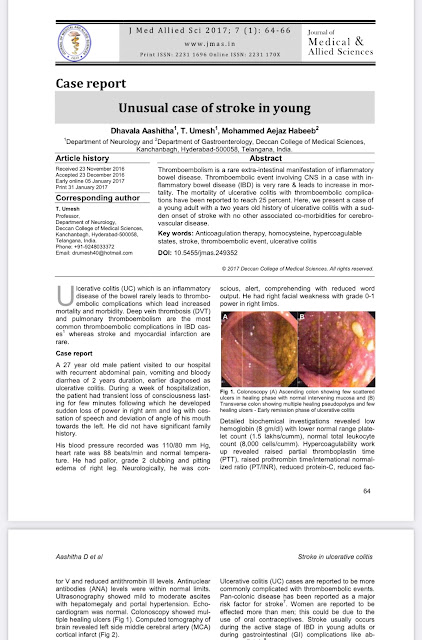
Speaker: Our publication in American Journal of Neurodegenerative diseases last year around 5 cases.
The first case was regarding a 50 year old man with progressive supranuclear palsy, the second one regarding corticobasal degeneration, the third case is regarding a parkinsons case who later developed auditory hallucination secondary to drug therapy, fourth case was regarding multisystem atrophy, fifth case was on a case with Alzheimer's dementia.
Thank you everyone
.jpeg)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)



.png)
.png)

.png)
.png)
.png)
.png)
.png)


.png)


.png)
.png)
.png)


Comments
Post a Comment